
Arthropathy is a chronic joint disease caused by metabolic disorders. As a result, degenerative, dystrophic changes and destruction of cartilage tissue occur.
It happens unknowingly, but usually develops very rapidly. A person begins to experience joint pain, stiffness, and reduced mobility when moving, especially in the morning, but remains "uncoordinated. "If discomfort and periodic pain occurs during clumsy movement or weight bearing, it is very important to understand that this will not go away and will only worsen without intervention.
Symptoms of joint disease
Arthropathy of the large and medium joints severely alters a person's lifestyle, worsens quality, and imposes limitations. The disease progresses like an avalanche, and treatment is often accompanied by excruciating pain, a telltale sign of joint wear and tear.
The symptoms of joint arthropathy depend on how much the joints, cartilage tissue, and nearby tissues are affected.
In the initial stage, arthropathy can be identified with a fair degree of accuracy, and treatment in this case is economical and does not require serious intervention and expensive drugs to treat arthropathy.
Types of Arthropathy
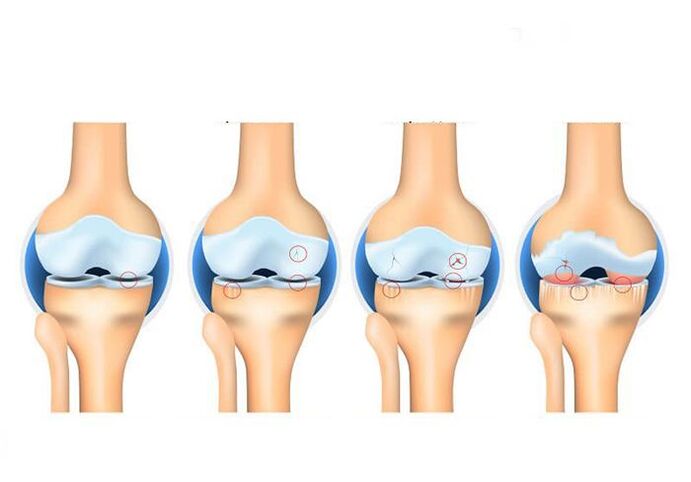
Arthropathy of the joints is classified according to several criteria. According to the degree of joint disease in the cartilage tissue, 4 stages of arthropathy can be distinguished. Arthropathy is also divided into primary and secondary. Primary arthropathy develops due to age-related changes. Secondary arthropathy occurs as a result of injury and disease to the joint (eg, traumatic arthropathy or rheumatoid arthropathy). The disease can also develop slowly over a few years or cause joint destruction (progressive arthropathy) in just a few years.
and alsoDepends on the type of joints in the affected area:
- – Knee Arthropathy – Hip Arthropathy
- Uncovertebral Arthropathy - Cervical Spondylosis
- Spondylosis - damage to the spine
- Patellofemoral arthropathy is a disease of the knee in which the patella and part of the femur are affected.
The degree of disease is determined by the degree of cartilage tissue damage.
1st degree joint - the cartilage tissue is slightly damaged and the person does not feel discomfort;
Arthropathy II degree - the appearance of osteophytes, the narrowing of the space between the cartilages, the situational pain with difficulty in movement;
Degree III arthropathy - partial destruction of cartilage tissue and exposure of bone tissue, narrowing of the space between cartilage, frequent and severe pain;
Degree IV arthropathy - vital parts of cartilage tissue are destroyed up to 60%, there are no gaps between the bones, the patient experiences constant severe pain, and hyperthermia occurs in the area above the joint.
- Tightness and mild background pain characteristic of exercise;
- Limitation of joint movement, discomfort when moving the whole body;
- "Jump" blood pressure indicator;
- headache and dizziness;
- Convulsive syndrome and frequent muscle cramps;
- Joint deformities observed with the naked eye;
- swollen, hyperthermic, or red areas of skin on affected joints;
- Violation of motor function.
Why does this disease occur
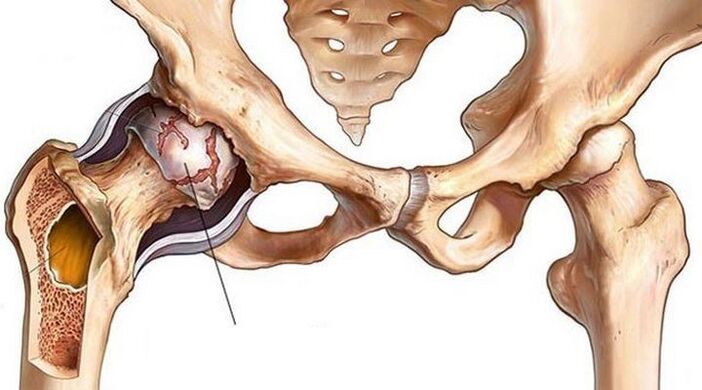
Arthropathy of the joints can manifest in any department, but most often the patient turns around when the joints of the knee or hip are present. In the professional field, the shoulder joint can be observed due to the special specific load on the hand.
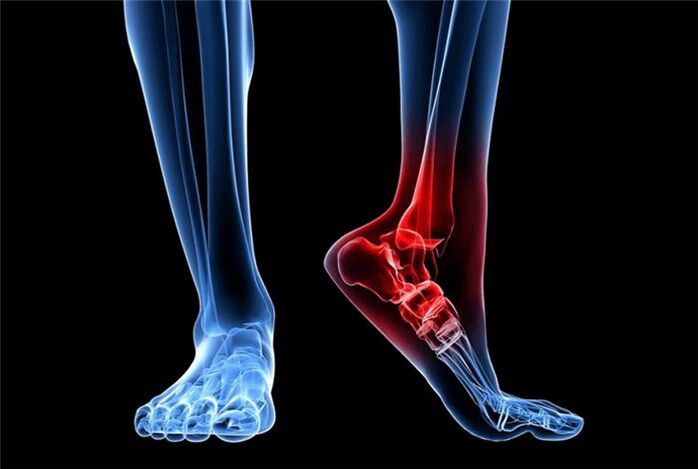
The lesions are different in men and women.The strong half often suffer from temporomandibular, wrist, ankle, and lumbar spondylosis. Women complained more about the chest and neck area, as well as the joints of the fingers and big toes.
The type of disease depends on the location of the lesion. There are the following:
- Arthropathy of the hip - arthropathy of the hip;
- Arthropathy of the knee - arthropathy;
- Injury to the patella and part of the femur - patellofemoral arthropathy (a type of joint disease);
- Diseases of the spine - spondyloarthropathy;
- Cervical spine injury - uncinate joint disease.
The main reason is:
- inflammatory process;
- professional sports;
- overweight;
- Professional non-standard weight bearing, such as squatting or kneeling;
- previous joint injury (post-traumatic);
- low temperature;
- hereditary;
- age changes.
Arthropathy can present as an independent disease or the result of a pre-existing disease, so it is important to know a person's medical history.
Diagnosis of joint disease
Arthropathy of the joints is detected by X-ray. X-ray images show how the joint is deformed and how narrow the joint space is. MRI or arthroscopy may also be required, but only in particularly complex and equivocal cases. Usually, an X-ray of the joint is sufficient to diagnose the disease.
A comprehensive diagnosis is required in order to understand the presence, severity, and disease causing the disease.
First, with helpX-rays in different projectionsReceive information about the extent of joint damage.
Tomography (magnetic resonance or computer) can helpTumor processes were excluded.
Third, you needTake the testFind out if arthropathy is a separate disease or a complication, and determine a person's general condition.
The complexity of the studies is most abundant and provides a clear understanding of the changes in degenerative malnutrition and helps to select the best treatment plan.
Treatment of joint disease
As mentioned above, arthropathy can develop due to a variety of factors, and treatment planning is based on an understanding of the underlying cause and selection of medications to treat arthropathy accordingly.
Treatment should be tailored individually based on the diagnosis. Be sure to take into account the person's condition, his existing disease.
The recovery of the articular surfaces and cartilage tissue is not quick. Prescribe effective medicines with side effects. The drug was taken for up to 6 months to achieve the desired effect. Therefore, it is important to protect your health from side effects as much as possible.
Drug therapy for joint disease
The main goal of this treatment is to eliminate the manifestations of arthropathy. Medications for joint arthropathy include:
- Non-steroidal anti-inflammatory drugs. With arthropathy, a person experiences pain and the joint becomes inflamed. To get rid of unpleasant symptoms and stop inflammation, this group of drugs is prescribed.
- Inject hormones into the joint. Corticosteroids are most commonly used in the acute phase of arthropathy.
- chondroprotective agent. The main task of these drugs is to stop the degenerative process of cartilage tissue in order to prevent its further destruction.
- Intra-articular injection of hyaluronic acid. The hyaluronic acid preparation is similar to synovial fluid and provides sliding and smooth free movement in the joint. With arthropathy, synovial fluid secretion is insufficient, so orthopedic surgeons often prescribe hyaluronic acid injections (injection into joints with arthropathy).
- Biological therapy of arthropathy (PRP and cytokine therapy). A new innovative approach to the treatment of arthropathy that has recently entered practice but is gaining popularity. This is based on the use of platelet-rich drugs in the patient's plasma. Thanks to the biological therapy, the blood supply to the joint is activated, the production of fluid in the joint is activated, and the cartilage tissue is nourished.
important!Drug therapy for arthropathy is effective in the early stages of the disease. In addition, experts stress that drug therapy cannot restore damaged joints, but it can eliminate symptoms and slow the progression of arthropathy.
Physiotherapy and Conservative Treatment of Other Arthropathy
Physiotherapy is also used in the fight against arthropathy. Various procedures (laser, ultrasound, electrophoresis, magnetotherapy, UVT) and exercise therapy are prescribed to improve metabolic processes and blood circulation, strengthen muscles.
Also, with arthropathy, you just need to make a few adjustments to your lifestyle:
- Avoid overloading - it is important to distribute activity and rest evenly to avoid overloading your joints
- Pay attention to nutrition and monitor your weight - since being overweight will only exacerbate joint problems, you need to revisit your diet and lose weight
- Remember to be careful and avoid injury as much as possible
- Use extra support for movement - In the later stages of arthropathy, independent movement becomes problematic, so you'll need to use crutches or crutches. To walk more comfortably, you can also use orthopedic insoles - they reduce the load on the joints.
There are also many folk recipes "helping to overcome joint diseases". However, treating joint disease at home does not always bring results. Also, using a variety of lotions and ointments that you make yourself usually only causes allergic reactions and doesn't affect the health of your joints.
Surgery for Osteoarthritis

How to treat arthropathy if none of the above methods work? In this case, surgery for osteoarthritis is required. Choose a type of surgery based on the degree of joint damage and the individual characteristics of each patient.
Arthroscopy is a low-invasive intervention, an intra-articular procedure performed through several micropunctures in the joint. For arthropathy, it is used as a temporary measure to "clean the joints": to remove parts of the cartilage, osteophyte growths that interfere with free movement. This treatment reduces joint pain, but does not solve the problem of arthropathy.
An osteotomy is an operation to align the axis of a joint. The truth is that with arthropathy, usually, one part of the joint suffers more (it has a lot of load). Due to the osteotomy, the load on the joint is redistributed. It should be noted that arthropathy is a progressive joint disease. Therefore, osteotomy is a way to delay further treatment, but not avoid it.
Joint replacement is an effective, and in some cases, the only way to treat joint arthropathy. The essence of the surgery is to remove the joint destroyed by the disease and implant an artificial prosthesis in its place. The artificial joints are individually selected, very suitable for each patient, and fully complement the function of the damaged joint after a period of rehabilitation.
Contraindications for Arthropathy
Things to watch out for in joint disease:
combined load- For arthropathy, you need to give up heavy lifting, excessive static loads. Joints can be unloaded using crutches. Shoes - Proper footwear can reduce stress on your joints. It is recommended to avoid wearing high heels.
weight- Being overweight is another factor in the progression of arthropathy. Therefore, maintaining a healthy weight and eating a balanced diet is important.
sportyReview is also required. For arthropathy, it is necessary to exclude strenuous exercise (contact sports, wrestling), long-distance running, weightlifting. But this does not mean that physical activity should be stopped completely. Moderate activity only benefits the joints.
In addition to medication, physical therapy is actively used. These are magnetic therapy, electrotherapy, hyperthermia. Additionally, physical therapy exercises are recommended to strengthen the muscles around the affected joints and improve blood supply.
The underlying approach to joint deformities that worsen quality of life is usually surgical intervention. In this case, arthroscopy or arthroplasty is performed.
Arthroscopy is a procedure to remove the worn top layer of the joint and place a partial prosthesis in its place. This allows you to get rid of pain and regain mobility.
An endoprosthesis is the replacement of a joint with a prosthesis. Applies to severe damage when the joint itself does not make sense to save. The prosthesis has artificial cartilage, which corresponds anatomically to human cartilage.
The initial treatment of the disease is to provide high-quality nutrition to the cartilage tissue. For this purpose, chondroprotective agents, preferably flavonoids of natural origin, are recommended. Exercise load is also necessary to improve blood supply to the bones and perichondrium.
Deformation of the knee
knee osteoarthritisGonarthrosis (DAK) is a chronic progressive disease of articular cartilage. It is characterized by destruction of the joint structure, accompanied by pain, inflammation, and characteristic bending of the limb ("leg on wheels" or X-shaped deformation).
Causes of Knee Deformation
Without proper lubrication, the joint can "dry", crack, and lose height, exposing the head of the bone. In this case, the closed plate of the articular surface of the bone remains defenseless; re-stimulation of the numerous nerve endings within it can cause pain and discomfort.
The following factors, or a combination of them, can be the cause of a deformed knee joint:
- Joint disease (especially knees) in relatives;
- Genetic disorders associated with abnormal, unstable chondrocyte formation or accelerated death;
- Congenital and acquired deformities of the musculoskeletal system (flat feet, joint hypermobility, dysplasia, scoliosis, kyphosis, etc. );
- Excessive professional, home or exercise load;
- Microtraumas and injuries of the knee and meniscus, surgery, leg fractures;
- Circulatory disorders (varicose veins, atherosclerosis, thrombosis and other vascular diseases), their consequences (anatomical osteochondritis) and other causes of long-term spasms in the legs;
- Inflammatory diseases of the joints and tissues around them (synovitis, bursitis, tendinitis, arthritis), including autoimmune (rheumatoid, psoriatic arthritis);
- Metabolic disorders (gout, diabetes);
- Age-related joint aging process and loss of calcium from bones;
- hormonal disturbances and changes in hormonal background (eg, associated with a lack of estrogen in women);
- vitamin deficiency;
- overweight (observed in ⅔ of patients);
- Physical inactivity.
But the main reason knee deformation is so common is its structure. The knee joint has only one axis of motion (plane). Therefore, the allowed range of motion is very limited. An awkward turn can damage the tissue around the joint and trigger joint disease—after all, a sore knee is subject to everyday stress.
The development of knee osteoarthritis can be due to many factors.

Symptoms of knee osteoarthritis
Gradually increase the pain in the knee area. At first, the pain is only noticeable when moving - for example, a feeling of "unfortunate footing" when the leg is sharply straightened or bent. In the early stages, pain may be occasional or mild enough to be considered discomfort. The pain then intensifies after physical exertion or prolonged holding in the same position. The skin can also become sore - it reacts sensitively to any touch, incl. and clothes.
There are 3 types of pain specific to knee osteoarthritis:
- Begin (15-30 minutes after the joint exits a prolonged rest);
- Mechanical (detectable during physical activity, disappears after rest);
- Blocking (feeling a sharp squeeze in the knee).
Symptoms of knee osteoarthritis usually grow slowly because the disease is not characterized by rapid progression. This is the insidious nature of arthropathy - gradually adjusting to the discomfort of the disease, the patient "gets used to" the pain, not noticing the worsening and delaying seeing the doctor.
Knowing the main symptoms of knee osteoarthritis can help to detect the disease in time
Treatment of knee osteoarthritis
Treatment of knee osteoarthritis involves complex use of medications, dose loading of the joint, physiotherapy procedures and the use of orthopedic devices.
During treatment, it is very important to alternate loading and unloading to prevent static loading of the knee joint. Orthopedic insoles, special shoes, walking sticks, crutches, walkers, and ergonomic chairs for work and rest also help slow the disease. Particularly effective are orthoses with variable reinforcements, which simulate the physiological axis of the leg and compensate for deformities.
In the early stages of knee deformity, the goals of treatment are to restore the damaged joint and ligamentous organs, reduce pain and increase the range of voluntary motion. Later - in relieving the patient's condition. For this purpose, hygienic arthroscopy (cleaning with antiseptic), corrective osteotomy (correction of bent bones), intra-articular prosthesis (replacement) is performed when a piece of osteophyte falls off.
In addition to orthopedists, physiotherapists and chiropractors, sports therapy and therapeutic massage specialists and surgeons will tell you how to treat knee osteoarthritis.
The treatment of joint deforming arthropathy is a complex and lengthy process that requires a comprehensive approach.

physiotherapy
Among other physical therapy methods for the treatment of osteoarthritis of the knee, the following are used:
- Laser and magnetic therapy;
- microwave therapy;
- shock wave therapy;
- amplify the pulse;
- ultrasound therapy;
- Perform electrophoresis with analgin, neocaine, chymotrypsin, etc. ;
- Acoustic therapy with glucocorticoids;
- Paraffin and ozokerite applications;
- cryotherapy;
- acupuncture;
- Combined traction and exercise therapy;
- Bath therapy.
Knee Deformation Joint Massage
Therapeutic and lymphatic drainage massage and manual therapy for the deformed joint of the knee by a specialist after the joint inflammation has resolved. For self-massage at home, stroking and rubbing are recommended, as well as exercises aimed at stretching muscles and ligaments, a deep warm-up (at the end, after the warming effect). Self-massage complements local stimulants and essential oils. Remember, with deformed knee joints, massage both joints even if only one of them is affected.
Knee Deformation Joint Exercises
Therapeutic gymnastics (kinesiology) for knee osteoarthritis is performed in a sitting or lying position, and water aerobics are also effective. A set of individual exercises developed by a trainer for deforming knee osteoarthritis. Below we provide a brief warm-up designed to strengthen the leg muscles.
- Sit on the floor with your legs straight and your hands behind your back. Bend and straighten your toes.
- Starting in the same position, slowly bend your legs, placing your toes on the floor at the end of the movement. Repeat with the foot behind the other foot.
- Continuing in the same starting position, bring the outstretched leg in front of you, with the toes facing you.
- Without changing the starting position, we pull our hands over the toes of the straight leg.
- Sit on the floor, hug your bent knee, and try to raise the other leg above the floor.
- Sit on the floor with your legs shoulder-width apart. Rotate your legs one by one so that your toes move 180 degrees.
- Sit on the floor with your legs bent. Roll your foot from heel to toe and feel the action on the back of your thigh.
Excellent! Do exercises for knee osteoarthritis at least 3-6 times a day.
Knee Deformation Drugs
Medications for knee osteoarthritis can quickly stop acute pain, reduce inflammation and swelling, and improve joint nutrition. Therefore, the drug is used in all stages of the disease to help restore the mobility of the knee joint.
chondroprotective agent
Chondroprotective agents in the form of tablets, capsules, sachets and injections are used to regenerate and maintain synovial cartilage.
Anti-inflammatory (medicine)
Steroid and non-steroidal anti-inflammatory drugs are used to treat osteoarthritis of the knee. They are prescribed in the form of tablets, injections, sachets, creams, ointments, and other topical and internal products.
Anti-inflammatory drugs can be used in combination with anesthetics, which are injected into the joint cavity as a blocker.
antispasmodic
Spasticity must be relieved to allow the patient to resume normal activities and normal supply of nutrients to the tissues.
Vascular protector
In order to deform the knee joint, a preparation based on horse chestnut or the like is used.
warming agent
Among the warming agents, preparations based on natural ingredients are worth highlighting: snake and bee venom, peppers, mustard.
All of these drugs improve blood supply to tissues and spread pain.
Nutrition for knee deformities
A healthy diet for deforming the knee includes dishes with reduced trans fat and "fast" carbohydrate content. Lean meats and fish, seafood and vegetables should be prioritized, steamed, foil-wrapped or stewed with a lid on. Also helpful are fruits, berries, and antioxidant-rich beverages -- wild plants, blueberries, lingonberries, cranberries, high-quality green tea and coffee. You can also eat whole grain cereals and beans.
But potatoes, white bread, candy, convenience foods, fast food and alcohol should be excluded.
If you are overweight due to a deformed knee, consider opting for a low-carb diet.

























